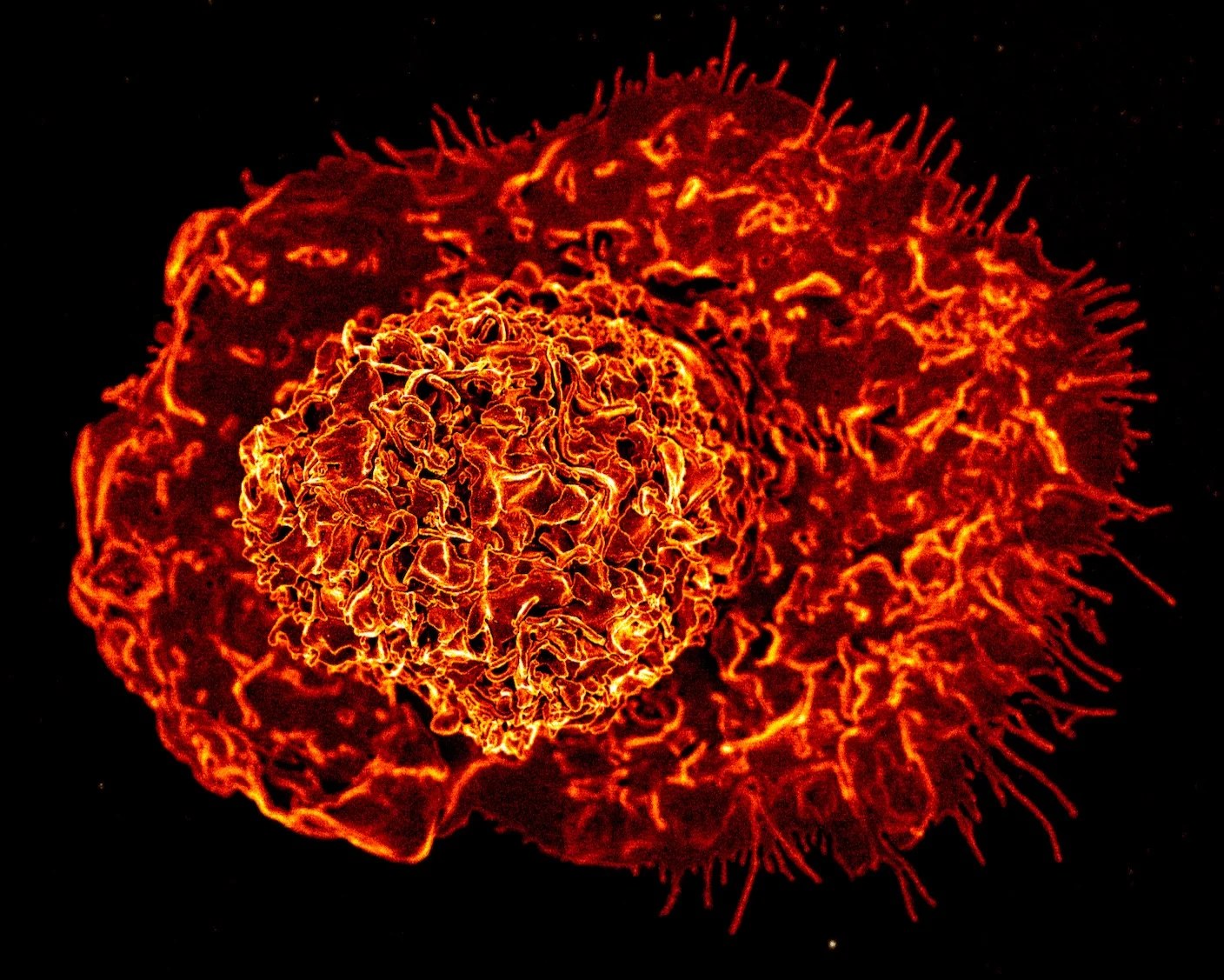
Macrophages—or “big eaters”—are exactly what they sound like. These immune cells roam our bodies hunting down infections, cancers, or injuries. When they detect a target, the cells release a calvary of signaling molecules that recruit other immune cells to mount a response.
More recently, scientists have discovered a sedentary offshoot of the family. Hidden in fthe nooks and crannies of the fatty tissue enveloping our organs, these macrophages differ from their roaming cousins. Little is known about them, other than the fact they come in a variety of types and seem to decline with age. Scientists have hypothesized they might help balance chronic inflammation during aging, but without knowing more, the idea is hard to test.
Now, a team from the Yale School of Medicine has painstakingly charted the family tree, sorting these fat-dwelling macrophages into 13 types. Several populations were already known, such as nerve-associated macrophages that, true to their name, hover near and connect to nerves.
Another group was completely new to science. These cells were virtually absent in young mice and only appeared in older ones, and they appeared to contribute to inflammation.
“We did not anticipate that there would be a completely new cell type,” study author Vishwa Deep Dixit told Nature.
The newcomer seems to engage in a tug-of-war with nerve-associated macrophages: The former increases inflammation and the latter douses the fire. With age, however, nerve-associated macrophages dwindle—and so too does their fight against inflammation.
The results suggest a tantalizing idea: Perhaps re-balancing the two cell types could combat chronic inflammation that occurs as people grow older.
The Macrophage Family
Fatty tissue macrophages are an odd bunch. Unlike their circulating counterparts, these cells don’t often detect or fight infection (although they can). Rather, their main job is housekeeping. They eat dead fat cells, reshape fatty tissues, and regulate metabolism.
The cells like to nestle in special niches inside white fat. Some hover near crown-like structures that contain dying fat cells, where they can find their next meal. Others cuddle up to blood vessels and scrub away dead cells. Still others—nerve-associated macrophages—latch onto nerves and regulate movement in the gut, trigger immune responses against flu viruses in the lungs, and regenerate nerves in the skin.
Despite having a range of beneficial occupations, little is known about what happens to each type as we age. To find out, the authors of the new study isolated fat macrophages from male and female mice aged the rough the equivalent of young adults and elderly humans. They analyzed the RNA landscape of each cell. RNA reflects gene activity as well as the cell’s overall health.
Thirteen RNA signatures popped up, each with its own quirks. But two were especially eye-catching.
One of these was linked to nerve-associated macrophages. The team found their numbers and RNA profile changed vastly with age, though the specifics differed between female and male mice. Although the cells are more abundant in young female mice compared to males, their numbers tanked in elderly females only. Those cells that remained became more inflammatory. They showed an increase in genes associated with senescence, a process where cells break down and leak a toxic pro-inflammatory soup that damages surrounding tissues. Some even harbored genes associated with late-onset sporadic Alzheimer’s disease.
Then there were the newcomers. These exhibited a unique signature not seen before. They amounted to only one percent of the fatty macrophage population in young mice. But that number shot up to 20 percent in elderly mice. A closer look at their RNA profiles found signs of senescence, along with pro-inflammatory genes related to cytokines—a type of immune molecule—and other proteins known to drive up inflammation.
Where and how these cells pop up is still a mystery. Though more study is needed, the team suggests the accumulation of the cells as we age could contribute to systems breaking down.
Double Duty
The team next took a closer look at nerve-associated macrophages in young mice under the microscope. The cells snuggled up to nerves in white fat tissue and extended “arms” that encircled the nerves. The macrophages expressed multiple genes encoding a nutritious protein related to growth and healing and seemingly cleaned up old and dysfunctional myelin—a fatty “wrapper” encapsulating neuron branches that’s critical for normal brain cell function.
This activity suggests they might help maintain nerve cells or support their survival, wrote the team. As the cells dwindle and become pro-inflammatory with age, the protective effect would likely go away.
Nerve-associated macrophages also have a hand in fat metabolism. Young mice genetically deprived of these cells showed increased inflammation in their blood, including higher levels of toxic cytokines and disrupted metabolism of fatty tissues, resulting in fat accumulation, which has been associated with aging. The cells seem to sit at the crossroads of inflammation, nerve health, and fat metabolism—all of which get out of whack as we age.
“Together, these data demonstrate that a reduction in [nerve-associated macrophages] during aging alters the immune cell landscape in VAT… and suggest that loss of [nerve-associated macrophages] may potentiate age-induced inflammation,” wrote the team.
While the study sheds light on these cells, the role of the newly discovered macrophage type is unclear. Where do they come from? What causes them to grow in numbers with age? Could wiping them out in the elderly reduce chronic inflammation? The team found a protein marker that identifies these cells and hopes it can help them decipher the cells’ role in chronic inflammation in future studies.
Source link
#Scientists #Newly #Discovered #Immune #Cell #Drive #Inflammation #Age